Previously published on fastradius.com on August 3, 2020
Medical devices are challenging products to manufacture. The combination of regulatory requirements and life critical components make the development expensive and technically difficult.
Stage 1: Ideation and Conceptualization
The first step to developing a medical device is identifying a user need in the target market. Minimizing the gap between the user’s needs and the designer’s perception of those needs is critical to creating a successful product.
Needs in the medical community primarily fall into two categories — “vitamins” and “painkillers.” “Vitamins” are not healthcare solutions, but they do support or improve patients’ quality of life. “Painkillers” are devices that directly address a medical problem.
To assess user needs, start with these seven key questions:
- What will the device do?
- Who is going to use it?
- When will it be used?
- What are the most important features to consider?
- How will the user use this device?
- What are the clinical indications/applications for the device?
- Is the device single-use or multi-use?
A strong development team is critical here — think experts in engineering and design, usability engineering, medicine, compliance, quality assurance, and intellectual property law. These partners will help answer these questions, ensure the concept is promising enough to pursue, and mitigate risk.
This stage is also the time to lay the groundwork for the rest of the medical device design, development and manufacturing process. This includes coming up with timelines for the project at large as well as its individual stages, calculating potential revenue, gathering an understanding of the regulatory pathway ahead, assessing risk, and budgeting. Budgeting considerations can include funds for labor, materials, consulting, product testing, clinical trials, biocompatibility testing, and licenses and fees if the product will be released internationally.
Stage 2: Regulation and Compliance
The second stage of medical device manufacturing is very involved, but is critical to ensuring only the safest products make it to market. Every medical device must pass regional and international compliance standards that ensure the quality and usability of biomedical tools, materials, and equipment.
For example, all product designers must heed the International Electrotechnical Commission (IEC) standard 60601-1 — it sets out the general requirements for medical electrical equipment and guidelines for health and safety.
However, compliance requirements are not all-encompassing. If a device is compliant with all IEC and International Standard for Organization (ISO) standards, that doesn’t necessarily mean that the Food and Drug Administration will approve it. The FDA has its own parameters for compliance that are derived from regional and international standards, to which engineers will also have to adhere. Finally, engineers must also consider design control regulations set out by the FDA. Design controls are the parameters an engineer uses to prove their product is safe, effective, and able to meet the needs of its target market.
Stage 3: Product Development and Design
Design is the most important stage of the medical device manufacturing process. Even if it makes it through regulatory compliances, a loosely defined or designed device can’t make it to market and deliver the functionality it promises.
The product development stage is oriented around design inputs and design outputs. Design inputs are the physical and performance characteristics that are used as the basis for the device’s design. Good design inputs are clear, objective, and written as provable or disprovable statements. Design outputs are any drawings, specifications, and manufacturing instructions that are associated with the device.
Engineers should keep copies of design inputs and outputs, plus the design plan — which includes a description of all development activities, who is responsible for said activities, and when design reviews will take place — and update them as needed. In conformance with regulations and good design principles, dated signatures need to be gathered by all responsible engineers during the design process.
As the technical capabilities of the device are being proven out in laboratory settings, product and industrial designers can begin to build the form of the device. Here, rapid prototyping will help engineers and designers move through several concepts. Once the technical aspects of the device begin showing repeatable results, a functional prototype can be built. This will start the process of replicating the scientific breakthrough seen in a laboratory setting in a less controlled environment.
Some considerations to discuss as the device moves out of the laboratory are:
- Precision — How will precision be measured? How will the device remain precise over time?
- Lifespan — How long will the device last? What happens when it must be fixed and how will that affect patient health?
- Travel limits — Will the device include any sensors or switches that limit mobility?
- Mechanical safety — Are there any pinching or crushing hazards?
- Debris — Will any debris from the device compromise user safety or biocompatibility?
- Fringe cases — What happens during worst-case scenarios?
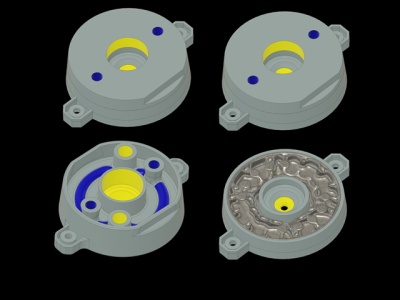
Additive manufacturing is a quick and cost-effective way to develop medical device prototypes, as no tooling is required. An experienced manufacturing partner can help product designers decide what material and manufacturing processes are best suited for a given part.
Stage 4: Testing
The testing stage is all about verification and validation (V&V). Verification is an internal process that evaluates whether or not the device meets the specified requirements, and confirms whether or not design outputs have met inputs.
Validation is an internal-external process that evaluates whether or not the device delivers on its promised benefits. The development team will need to enlist a medical technology expert to help create the tests used for V&V to ensure the tests are as comprehensive as needed.
Since no device turns out perfect on the first try, the testing stage can quickly put product teams over-budget. A strong test strategy can optimize costs and help engineers get their products to market at speed.
Get Started With SyBridge
The medical device manufacturing process is like a waterfall, not a step ladder. Engineers should expect to progress from one stage to the next as well as frequently cycle back through previous stages based on ongoing feedback. In every stage of medical device design and manufacturing, product teams can benefit from the advisory of a trusted manufacturing partner.
At SyBridge, we’re passionate about creating a better world by helping product teams of all shapes and sizes create products that improve the health, safety, connectivity, and sustainability of our world. Now more than ever, high-quality medical devices are a large part of that. Our dedicated team of designers and engineers can provide end-to-end support on product design, material selection, manufacturing method, finishing and post-production, and more. We’re dedicated to helping product teams like yours make new things possible. Contact us today.